Employee mental health issues are on the rise. And. Are increasing yearly.
Leaders now face huge challenges regarding mental health in the workplace.
What to do? How to tackle this problem? Do they, in fact, have the skills necessary to address employee mental health challenges?
Are EAP’s (Employee Assessment Program – re mental health issues) helping solve these mental health challenges in the workplace? Why are employees afraid to opt in to these programs?
Have leaders relegated the issue of employee mental health challenges to the too hard basket? Or, in fact, do they think that by having an EAP in place, abrogates their responsibility to their employees, especially when the uptake rate by employees is between 5 -7 %?
Are they, in fact, missing the point entirely on these issues?
Is the necessity to find a quick solution, shifting the focus on what the real causes of employee mental health are?
Simply having posters and discussions on issues such as depression and anxiety – an awareness campaign – is that sufficient?
To me, the answer is: No.
If leaders and employers can gain a more comprehensive background as to the nature of the real causes of employee mental health issues, why it arises, and where it comes from, they will then be better informed as to how to deal with those employee mental health challenges in the workplace.
In this guide, my aim is to give you that broader perspective, so that real change can be implemented. I am talking about more natural and more healthy approaches which can be implemented to alleviate employee mental health issues in the workplace, in as little time as possible.
Table Of Contents
- Definitions: Mental Health, Employee Mental Health, and Other related terms.
- What are the Signs and Symptoms of Employee Mental Health Issues?
- Background: The History and Concentration of Ideas on Employee Mental Health as per the WHO Organisation and American Psychiatric Association
- Most Common Types of Employee Mental Health Issues in the Workplace- Anxiety and Depression Disorders
- Research and Evidence of Factors Exacerbating Employee Mental Health Issues in the Workplace
- Common Solutions for Employee Mental Health Issues Used in the Workplace– The Traditional Approaches – Psychiatry v Psychology
- A New Perspective on Dealing With Employee Mental Health Issues in the Workplace – Let’s Talk About Stress reduction
- A New Solution: A Five Step Stress Reduction Plan for Leaders to Help Employees Deal with Mental Health Issues in a More Comprehensive Way
- Some Commonly Asked Questions on Employee Mental Health such as: What causes mental illness; Can mental health go away… and other questions?
- A Challenge to Leaders: Implement Real Change on Employee Mental Health Issues or Continue Following the Pack?
1. Definitions: Mental Health, Employee Mental Health and Other related terms
Mental Health is an extremely difficult topic to tie down to one simple definition due to the fact that there are so many branches and types within those branches.
Mental Health Disorders as defined in Wikipedia: …” are classified as a psychological condition marked primarily by sufficient disorganisation of personality, mind and emotions, to seriously impair the normal psychological, and often social functioning, of the individual”

They go on to state: … “Individuals diagnosed with certain mental disorders can be unable to function normally in society…. Mental disorders occasionally consist of a combination of affective, behavioural, cognitive and perceptual components.”
Employee mental health issues specifically relate to issues such as depression and anxiety, which, if present in the workplace, can significantly affect productive functioning in that workplace because primarily, a person’s focus, concentration, mood and behaviour has been comprised.
The American Psychiatric Association states that generally illness called mental health disorders include: disorders that affect your mood, thinking and behaviour
Examples of these disorders include: depression, anxiety, psychoses, eating disorders, PTSD, addictive disorders, borderline personality disorders and schizophrenia.
So, the overriding factor for a state to be classified as a mental health issue is that the initial signs are on-going and continue to cause or exacerbate stress, and affect your ability to function. There appears to be an arbitrary time period of at least two weeks, before an issue is reclassified.
2. What are the Signs and Symptoms of Employee Mental Health Issues?
In order to be able to define issues as mental health issues the following types of signs and symptoms need to be present:
- Feeling sad or down
- Having confused thinking or reduced ability to concentrate
- Having excessive worries or fear, or extreme feelings of guilt
- Withdrawing from friends and activities
- Having significant tiredness, fatigue, low energy or problems sleeping
- Having delusions – detachment from reality, paranoia or hallucinations
- The inability to cope with daily stress problems
- Having trouble understanding or relating to situations and people
- Substance or alcohol abuse to excess
- Major changes in eating habits
- Loss of sex drive
- Experiencing excessive anger, hostility or violence
- Having suicidal thoughts
These types of thoughts and feelings can manifest as physical problems such as: stomach pain, back pain, headaches, or other unexplained health issues.
The APA goes on to explain that generally most mental illnesses don’t improve by themselves. They are very big on getting treatment if the signs and symptoms persist.
The new information indicates that in order to gain a better understanding of the pervasive nature of mental health issues, we now need to take into account these traits: hereditary, environmental exposures before birth and brain chemistry.
Inherited traits: it appears that if your blood relatives have had mental illness then there is a possible to link to current issues. There may be genes that affect this. And. The environment into which you are born may also trigger these effects.
Environmental exposure before birth: if the mother has had exposure to alcohol, toxins, drugs, have diminished nutrition, inflammatory conditions and environmental stressors have also been linked to mental health issues.
Brain chemistry: when neural networks in the brain are impaired, the function of receptors and nerve systems, and the information flowing throughout the body/mind become distorted, thus leading to incidences of depression and anxiety.
The APA also goes on to talk about the risk factors that may be an indicator of those people who may have an increased propensity to be influenced by these factors:
- A history of mental illness – generally in a blood relative
- Stressful life situations – divorce, loss of a loved one or severe financial problems
- An ongoing health issue
- Traumatic work place experiences such as in the military
- Excessive use of alcohol or drugs, and prescription drugs
- Childhood environmental factors – a history of abuse or neglect
- Limited social contact with friends or relationships
- Or having had a previous mental health issue
The long term issues that may flow from having a mental issue is that these can lead to a disability. It has been said that untreated mental illness can cause severe emotional, behavioural and physical health problems.
The types of complications that can arise from these untreated mental health issues include:
- Unhappiness and decreased enjoyment of life
- Family conflicts
- Relationship difficulties
- Social isolation
- Continuing use of tobacco, alcohol or drugs
- Intermittent periods of missed attendance
- Isolation can lead top legal and financial problems
- The can lead to poverty and homelessness
- Having these issues can lead to self-harm and self-punishment, or to suicide or homicide
- Decreased immune function can lead to increased infections
- These issues can also lead to heart disease and other medical conditions
How to prevent mental issues from gaining traction.
Pay attention to warning signs: go see a doctor or a therapist. Speak to friends and family.
Get regular check-ups: being knowledgeable of how you feel and taking action for self care is important.
Getting help when you need it: the issue with this is that sometimes it is hard to distinguish mental health symptoms from other physical symptoms.
Take good care of yourself: this includes eating well, getting sufficient sleep, regular physical activity and so on.
3. Background: The History and Concentration of Ideas on Employee Mental Health as per the WHO Organisation and the American Psychiatric Association
“Mental health must be an integral part of universal health coverage.”
Dr Tedro Adhanom Ghebreyesus – Director General, World Health Organisation
The United Nations, through a subsidiary, the World Health Organisation, has taken up the issue of mental health, from a slightly difference perspective than the rest of the world. The WHO is dedicated to the health, wellbeing and the rights of individuals. This “human rights” slant directs their overriding policy and universal health coverage initiative.
WHO has indicated that mental health issues have contributed to:
- Poor health outcomes
- Premature death
- Human rights violations, and
- Global and national economic loss.
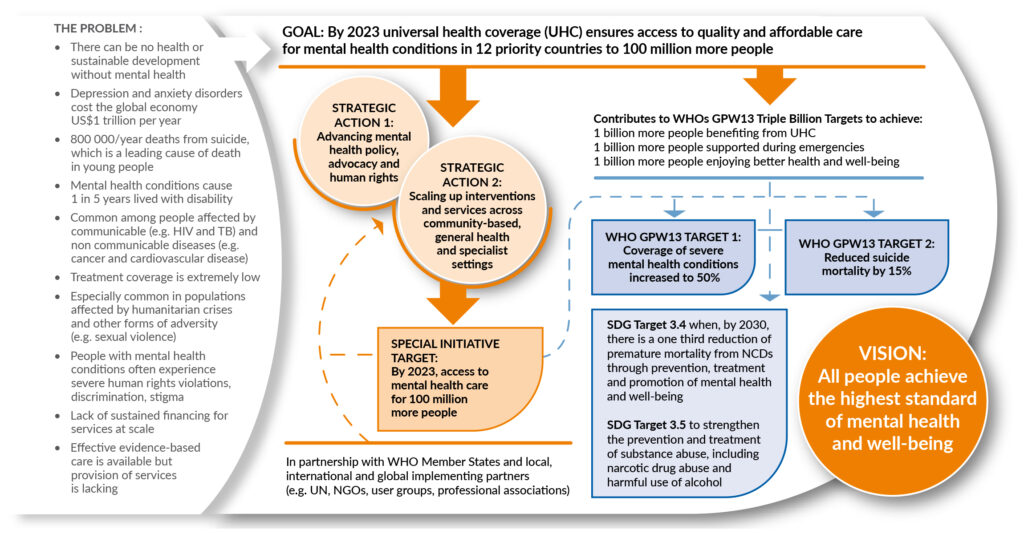
Due to that particular slant the WHO has instigated a Special Initiative for Mental Health for the years 2019 – 2023. In this document it is very hard to find a clear definition of mental health.
However, it goes on to state that: “Health is a state of complete physical, mental and social wellbeing, not merely the absence of disease”. So, from this they take a broader perspective, to include human rights elements.
“People with mental health conditions experience widespread human rights violations, discriminations and stigma.”
Without a clear-cut definition of mental health issues, they go on to describe what might be included as mental health issues: neurological and substance use disorders, suicide risk and associated psychological, cognitive and intellectual disabilities.
They then describe some of the more common types of mental health issues: depressive disorders and anxiety disorders, stating that these types of disorders impact mood and feelings of the affected persons.
WHO then outlines that the risk of becoming depressed, is increased by these factors: poverty, unemployment and life events such as death of a loved one, breakups, illnesses, or drug and alcohol abuse.
It is generally accepted that the most common types of mental health disorder prevalent within the workplace include: depression and anxiety.
To reiterate, the signs and symptoms to look out for include:
- Sadness
- Loss of interest or pleasure
- Feelings of guilt or low self esteem
- Disturbed sleep or appetite
- Poor concentration
The whole point about definitions of depression is the degree of the severity of the symptoms, and how long they last, and whether these symptoms are recurring. It has been said that if symptoms last longer than 2 weeks then there may be a problem. It has also been said that severe depression can lead to suicide.
Since mental health challenges are now a world-wide phenomenon, you might ask: “When did the recognition and treatment mental health commence?”
This helps establish the framework on which to assess the status quo.
Hippocrates, in the 5th Century BC has been given the title of pioneer in the field of treating mentally ill people. It has been said that he used these types of approaches:
- Changing the person’s environment
- Changing their occupation, or
- Administering substances as medications
Throughout history mental disorders have been presumed to have developed from:
- The supernatural
- Biological issues, or
- Psychological issues
Mental health issues were considered to be deviant behaviour, the internal battle between good and evil.
Various countries attributed mental health disorders to the Gods, the devil, biological or psychological issues.
The Bible alludes to the fact that these issues arise due to problems in the relationship between God and the individual. Quite often this was described as being possessed and therefore God’s protection was withdrawn.
This led to all kinds of treatment such as: blood letting, purges, whipping, exorcism, confinement, and eventually euthanasia in Nazi Germany.
During the 19th Century it became known that those who had mental health disorders also had physical and organic problems.
Over time it became a natural process of evolution that these types of disorders began to be classified. It became clear that there needed to be a separation of mood disorder from other psychoses, such as schizophrenia.
These developments were occurring at the same time various branches of therapy developed: psychoanalysis, clinical psychology and social work.
In the early 1900’s mental health disorders were called mental health issues.
World War II saw further developments due to the need for looking after soldiers. This led to the development of the psychiatric manual for categorising mental disorders. The Diagnostic and Statistical Manual of Mental Disorders.
Initially the majority of patients were housed in asylums. However, gradually private patients sought help.
In the 1930’s the term “stress” using a broad biopsychosocial approach, was increasingly linked to mental disorders.
Further treatments evolved during this time: lobotomies, insulin shock therapy, electroconvulsive therapy and neuroleptic chlorpromazine, therapies.
As mental health disorders became more prominent and non-institutionalised, the use of psychiatric medication became more prevalent. Initially this medication was called “psychic energiser”. Later lithium and bezodiaprines were used.
From the 1970’s, mental disorders not classified within the psychoses’ families, disorders such as depression and anxiety, were treated with cognitive behavioural therapy. This led to a new type of drug SSRI – antidepressants.
The American Psychiatric Association, having developed the DSM Manual to help categorise mental health disorders, underwent an overhaul and published the DSM-5 in 2013. It was stated that various criteria used to classify different mental disorders needed to be be overhauled.
During the early development of the DSM the term “reaction” was reflected. This was via the influence of Adolf Hitler’s psychobiological view that mental disorders represented reactions of the personality to psychological, social and biological factors.
It seems that the classification of the different types of diseases developed more out of the need for the Bureau of Census for gathering uniform health statistics across mental hospitals than any other reason.
In the 1880’s there were seven categories: mania, melancholia, monomania, paresis, dementia, dipsomania and epilepsy.
The WHO has been involved in the getting of information and educating people on the issue of mental health. They engaged many researchers and came up with a human rights approach. They state that people who have mental health issues experience widespread human rights violations.
Their findings include that persons from lower socioeconomic dispositions or countries experience greater hardship and mistreatment.
WHO found that within the most common or prevalent mental health disorders were: depression and anxiety. Their research indicates that depression has increased by 18.4% between 2005 and 2015. And. Anxiety has increased by 14.9% during that time period.
From there the most recent development included the Universal health Coverage for Mental Health 2019– 2023. The objective of this initiative is that companies world-wide will adopt these measures described in that Action Plan.
This WHO Action Plan has 4 major objectives:
- More effective leadership and governance for mental health
- The provision of company, integrated mental health and social care services in community-based settings
- The implementation of strategies for promotion and prevention of mental health issues
- Strengthened information systems, evidence and research.
From all of historical perspective and in more recent times the Australian Psychological Society did a five-year study from 2011 – 2015 on the mental health of Australian workers. (The following figures are cumulative.)
That anxiety is on the increase in Australian workplaces and that 87% of Australian workers are depressed either: mild, medium or severe, the severe category representing 26%.

It has also been shown that even though companies have implemented EAP’s (Employment Assessment Programs) the uptake of these services by employees is only between 5-7%. You have to ask why this is so?
Since then other issues have become more prevalent in the workplace such as: sexual harassment, bullying, racial or religious slurs, incidents of domestic violence, substance abuse and addictive behaviours and PTSD.
For the purposes of keeping this article within a shorter framework we will only concentrate on the most common issues: depression and anxiety.
In summary: mental health issues have been recognised throughout time and have been treated variously. The issues have become so widespread that the WHO, a branch of the UN, has conducted research and developed policies that they encourage employers to implement.
Common diagnoses criteria have been developed so that easier treatment options can be used. It has been found that even though there are clearer diagnoses, greater access to treatment options, increased education and awareness in the workplace, mental health issues are on the increase.
4. Most Common Types of Employee Mental Health Issues in the Workplace- Anxiety and Depression Disorders
The WHO organisation also agrees with naming these two disorders as the most common in the workplace: depression and anxiety.
The American Psychiatric Associations definition of mental health includes these points:
- These issues are characterised by a combination of abnormal thoughts, perceptions, emotions, behaviour and relationships problems with others.
- The types include:
- Depression
- Bipolar affective disorder
- Schizophrenic and other psychoses
- Dementia
- Intellectual disabilities
- Developmental disorders such as autism
The definition of depression coincides with the WHO definition. However, the APS goes on to state that “people with depression may also have multiple physical complaints with no apparent physical cause.”
The concern is about people’s ability to function at work or elsewhere, and to cope with daily life.
It was found that even though there are clearer diagnoses, greater access to treatment options and increased education and awareness in the workplace, mental health issues are on the increase.
Depressive disorders can be broken down into two categories:
- Major depressive disorders or episodes – includes a depressed mood, loss of interest and enjoyment, and a decrease in energy. Therapists then classify these as either mild, moderate or severe; or
- Dysthymic – which is a persistent or chronic form of mild depression, and which includes the above symptoms but tends to be milder, yet lasts longer.
Anxiety disorders include fear and are based on notions of:
- Generalised anxiety disorders
- Panic disorders
- Social anxiety disorders
- Obsessive compulsive disorders
- Post traumatic stress disorders ( PTSD)
In depressive disorders the biggest impact on the body/mind is on the mood or feelings of affected persons.
These following symptoms can range from mild to severe.
The characteristics of depression include:
- Sadness
- Loss of interest or pleasure
- Feelings of guilt
- Low self esteem
- Disturbed sleep or appetite
- Tiredness
- Poor concentration
It has been suggested that you can also have multiple physical complaints with no apparent physical cause.
Depression can be short term, recurrent or become a long term issue. The main point being that this disease can substantially impair a person’s ability to function at work or elsewhere, and impair their ability to cope with daily life.
It is indicated that depression can be managed with either therapy such as Cognitive Behavioural Therapy or psychiatry or psychology. And/or with anti-depressants. This is recommended for medium to severe issues. However, with mild depression, other therapies are recommended, which include helping the person identify the stressor triggers, and addressing them specifically.
Ok. So, for the workplace, these issues have been indicated as the types of behaviours that employees might exhibit, the identified risk factors which may affect employees, and that these types of behaviours may stem from a multitude of sources:
- The ability to manage one’s thoughts
- Emotions
- Behaviours
- Interactions with others
And these behaviours can stem from:
- Social
- Cultural
- Politic and environmental factors
- National policies
- Social protection
- Standards of living
- Working conditions
- Community support
- Stress
- Genetics
- Nutrition
- Perinatal infections
- Exposure to environment hazards
- Personality
- Biochemistry
- Exposure to:
- Violence
- Neglect abuse or poverty
It has been said that “all”, in some way, are contributing factors to employee mental health disorders.
Whoa!
This is an outrageous list of possible causes of mental health disorders for company leadership to become responsible for. How can a company possibly be responsible for an employee’s reaction to any one of these things let alone a several of them? What happened to personal responsibility? Are we now breeding a fragile type of human?
Okay. So, if this list is to eb taken seriously, there must be some hidden, underlying issue that is triggering a reaction to these personal or internal/external events.
From my observation and experience ALL of these types of issues can be caused by stress and can cause a stress reaction, a reaction that is visible mentally, emotionally, physically or spiritually.
To my mind, closer attention needs to be paid to these internal triggers, otherwise, from the above extensive list, we are all in serious trouble. This means leadership now needs to address an individual’s external personal life for possible risk factors that may trigger stress issues.
Depression
From my observation and experience depression signifies that a person constantly goes back into the past and tries to relive and change the outcome. The types of words used include: “if only I had….” This keeps them stuck in the loop and further suppresses the truth coming out. The person will not be able to address the issues when this happens. In fact, they will be in a constant state of denial.
This creates a constant loop of disappointment, knowing that the situation cannot be changed, but still willing and wanting that situation to change.
This is what creates the loop. This is what creates the release of unhappy chemicals and hormones flooding the body/mind. When you keep doing that, the body/mind gets stuck in a synapse, that guarantees that you approach all stress or disappointments in a similar way. This then reinforces the feelings of depression and contributes to the person maintaining that position.
My experience is that when people become depressed, they try to alleviate those feelings and escape for a time. They may: smoke, drink alcohol, ingest a lot of sugar or take medication or drugs.
The initial high is short lived and if you are prone to being trapped in those depressive feelings, when the high wears off, the let-downs are worse. All of these antidotes are of a depressive nature and make depression worse.
Why?
Because the person is further supressing their feelings, not being able to express them, and the drugs, the addictive substances pushes those feelings down further.
So, in essence, depression is about suppression of expression of feelings. Not being able to express yourself at your core. You then lose touch with your soul, your inner core, your identity, who you are and this leads to a depletion of passion, and a loss of identity, and life purpose.
So, the key is to get to those issues that have initiated this non-expressive behaviour and eliminate that, so that healing can take place.
And. Why don’t people seek help? It has been said that the types of barriers to effective care include:
- A lack of resources
- Lack of trained health-care providers
- Social stigma
- Inaccurate assessments
- Misdiagnosed and treated with antidepressants instead of something less radical
A personal case study, in point here.
I have been to doctors and told them about a stomach issue that had been hanging around for over two years and which included diarrhoea. They told me it was in my head and tat I was depressed and offered anti-depressants instead of trying to get to the real cause of the stomach problem.
Mistreatment by doctors and misdiagnosis can exacerbate ill health and this can lead to depression. Why? Because intuitively, I knew that depression was not the problem and that there was a real underlying cause of this stomach issues. However, because they could not align my symptoms with what they knew, they decided to classify me as being depressed. And. That is was in my head.
Health issues can lead to depression. Why? Because depression affects how you feel, the way you think and how you act. The medicos indicate that symptoms need to be in place for at least two weeks. However, conditions such as: thyroid, brain tumours or vitamin deficiencies can mimic symptoms of depression. Especially in women. Misdiagnosis can exacerbate ill health. This means that the patient need to be treated holistically, with emphasis on the physical as well and the emotional and mental aspects.
We know that in times of loss, sadness and grief, it is normal to feel down or depressed.
In grief, sadness and painful feelings come in waves. Yet your self-esteem can be maintained. Whereas in depression, the feelings of worthlessness and self-loathing eventuate. Death of a loved one can bring on major depression. Large or significant events can bring on major depressions. Death, divorce, loss of a job, loss of money, loss of health and son can also be pre-cursors to depression.
Anxiety
With anxiety, my observation and experience indicate, that this type of disorder stems from people trying to control every aspects of their lives. The more they try to control the more they see and get overwhelmed. The words used include: “what if this or that happens…”
Anxiety is a reaction to stress. It involves excessive fear about outcomes. Is it about anticipation of a future concern? It is associated with muscle tension and avoidance behaviour.
To be diagnosed with anxiety a fear must be out of proportion to the situation or age appropriate and must hinder the person’s ability to function normally.
There are various categories of anxieties:
- Generalised anxiety disorder
- Panic disorder
- Specific phobias
- Agoraphobia
- Social anxiety disorders
- Separation anxiety
The most common type in the workplace is: generalised anxiety disorder. It involves persistent and excessive worry that interferes with daily activities. This excessive worry can create these types of physical responses:
- Restlessness
- Feeling on edge
- Easily fatigued
- Difficulty concentrating
- Muscle tension
- Problems sleeping
The worries can be about anything e.g. job responsibility, family, health, car repairs, little things.
From my observation and experience an anxious person is someone who feels out of control and is hence constantly trying to control their environment. The more they try to control the more they see that is beyond their control.
The symptoms of anxiety include:
- Palpitations/pounding hear/rapid heart rate
- Sweating
- Trembling or shaking
- Feelings of shortness of breath/smothering sensation/choking
- Chest pains
- Feeling dizzy/light-headed or faint
- Feelings of numbness or tingling
- Chills or hot flashes
- Nausea or abdominal pains
- Feeling detached and fear of losing control
- Fear of dying… and so on
The APA in US state that the causes of anxiety disorders are currently unknown, however, they are likely to involve a combination of factors including:
- Genetic
- Environmental
- Psychological and
- Developmental
It has been noticed that anxiety can run in families.
Therapies include: talk therapy and medications. The types of medication given cannot cure but can give a person a significant relief from symptoms.
The types of medications given are: anti-depressants or beta blockers. People also recommend stress management techniques.
In the workplace we are interested in helping people with mental health issues. So, various organisations have instigated awareness campaigns and have put up several signs of mental illness outlined, such as:
- Sleep or appetite changes
- Decline in personal care
- Mood changes/rapid shifts
- Withdrawal (social, or loss of interest in activities previously enjoyed)
- A drop in productivity/functioning (failing in tasks, underperforming)
- Problems thinking/concentrating/memory/logical thoughts, or in speech
- Increased sensitivity
- Apathy – loss of imitative/desire to participate
- Feeling disconnected/ a sense of unreality
- Illogical thinking/exaggerated beliefs about personal powers
- Nervousness/fear or suspiciousness
- Unusual behaviour
So, with workplace mental health issues this is about having more than one of these symptoms at once, and that these combined symptoms are causing serious ability to function in daily life.
In summary: the most common types of employee mental health issues dealt with are: depression and anxiety. The problem appears to be that the majority of people in the workplace are depressed or anxious anyway, so this means that the approaches used to help employees, is far from adequate.
We will now look at these common solutions to gauge why this is so, and how best to implement e new approach.
5. Research and Evidence of Factors Exacerbating Employee Mental Health Issues in the Workplace
The first study alluded to earlier, was a series of annual assessments from 2011 to 2015 inclusive by the Australian Psychological Society into the effects of stress on Australian workers.
There were three main findings relevant to this expose:
- 87% of Australian workers are either depressed, suffer from distress or have anxiety issues, from mild through to moderate or severe.
- 50% of Australian workers feel that their employer does not care about their mental wellbeing, and
- 50% of workers also say that they do not feel that their employer values their contribution.

So, you can see here a workplace environment not conducive to helping make employees feel safe enough to mention their mental health issues.
Safe Work Australia’s study on Mental Health Costs on Australian Business indicates that is it costing Australian business over $10B per year, and that the highest claims were related to stress issues. They go on to say that mental health claims are the most expensive form of workers’ compensation claims.
Leading executive, Ms Sherry made this comment: “These findings highlight why it is necessary for employers to be aware of stress-related issues and improve current work practices to decrease unnecessary stress in the workplace.”
A further study by Andrew Noblet, 2017, Oxford University Press titled: Building Health Promoting Work Settings: Identifying the Relationship Between Work Characteristics and Occupational Stress in Australia, highlights this issue:
“Occupational stress is a serious threat to the health of individual workers, their families and the community at large. “
They go on to say: “Chronic occupational stress is regarded as both a serious public health concern and a major impediment to organisational success.”
For organisations, this occupational stress can contribute to a number of outcomes which are critical to organisational success, including:
- Absenteeism
- Labour turnover, and
- Job performance
Further results include:
- Lack of control over job/autonomy
- Support from work sources, and
- Unrealistic deadlines
…. were significant predictors of both psychological health and job dissatisfaction.
A Study by Medibank Private – August 2008 – titled: The Cost of Workplace Stress in Australia, concurred with the results above and added that 3.2 days per worker are lost each year through workplace stress.
And. That the number of stress related claims almost doubled between 1996 and 2004.
So, you can see from these few studies that there is a real workplace issue here. Stress is the number one contributing factor to employee mental health issues in the workplace.
One of the issues around mental health that confound people is that mental health does not suddenly appear. It does not spring out of nowhere. There are triggers. When the triggers and the resulting effects can no longer be ignored, the body/mind reacts physically, mentally and emotionally.
Because of this lack of understanding and acknowledgement that stress is the basis of ALL dis-ease and disease. (See the work of eminent biologist: Dr Bruce Lipton, in The Biology of Belief, where he states that up to 95% if all disease is self-created. The other 5% you are born with.)
This then means that you, the employee, create your mental health issues due to the stress your body/mind is subjected to on a daily, on-going basis. And. That if you do not treat or release or deal with those stress trigger issues, and, the resulting outcomes on your body/mind, you will zoom on by to disease, in the long run.
So, if this is the case, and the evidence is in on stress, as the major contributor to employee mental health issues, why aren’t employers viewing mental health solutions from this different angle?
In summary: there are many studies world-wide that show that workers are suffering from stress-related issues. There does not appear to be general consensus that these stress issues are really mental health issues, couched in different words. The key for leaders is to be aware of these findings, and then implement strategies, to overcome these stress-related, mental health issues.
6. Common Solutions for Employee Mental Health Issues Used in the Workplace– The Traditional Approaches- Psychiatry v Psychology
Due to the increasing number and types of issues identified, practitioners have found it necessary to have these mental health issues classified so that appropriate treatment can be ministered.
The led to the development od the DSM-5 (latest version) – The Diagnostical and Statistical Manual of Mental Disorders. This manual is about facilitating an objective assessment of symptoms which a person presents with, into a variety of clinical settings.

There are 3 major components of the DSM:
- The diagnostic classification (includes codes)
- The criteria set – is about symptoms (how long + conditions)
- And the descriptive tests.
The main point with this DSM is that there is no objective test to assess whether a person has any one of these particular disorders. It is all guess-work, however qualified the guesses may be. This means that a person could be assessed and ordered to take psychotic drugs (for life), and or be institutionalised, simply by the results of a subjective assessment.
The APA does say that it may be difficult to determine which disorder you may have. But that hopefully, with careful assessment by your health practitioner, a suitable classification can be made.
In the workplace an approach was identified, and rather than have practitioners (generally psychiatrists or psychologists) come into the workplace and identify individuals, a program called: Employee Assessment Program (EAO) has been instigated and adopted by most large and medium companies.
The employers and instigators of these EAP’s felt that the confidential nature of these types of programs would allay fears of employees of being disadvantaged.
A General Plan of Treatment for mental health issues, such as the following, is recommended:
- Your family doctor
- A nurse practitioner
- Physician assistant
- Psychiatrist, – a medical doctor who diagnoses and treats mental illness
- Psychotherapist, a psychologist or counsellor
- A pharmacist
- Social worker
- Family members/friends/support groups
Psychiatry is a branch of medicine focused on the diagnosis and treatment and prevention of mental, emotional and behavioural disorders. These types of doctors are qualified to assess both the mental and physical aspects of psychological problems.
They use both physical and psychological tests to get the whole picture of a person’s history and to assess the presenting symptoms. They then determine a treatment plan based on that clinical diagnosis. These doctors can prescribe medications. The medication s used are to help correct imbalances in brain chemistry that are thought to be involved in some mental disorders
Psychotherapy is “talk” therapy. The objective here is to eliminate or control disabling or troubling symptoms so the patient can function better. The number of sessions varies and these sessions can be one-on-one or in groups.
The types of treatment depend on the presenting issues. It could be about changing behaviours, thought patterns, exploration of past relationships and experiences, thus trying to help the patient cope with everyday situations by recognising behaviour and then being able to change this behaviour or modify it. These psychologists do not prescribe medications. The objective of cognitive behaviour therapy is focused on solving problems,
The types of medication recommended include:
*A warning comes with the use of these types of drugs and that is that they do not cure anything. But that they may make other treatments more effective, and they may help reduce the symptoms of mental illnesses.
Antidepressants. These are used for depression and anxiety and sometimes other conditions. It is said that these are not addictive and do not cause dependency. They can help improve symptoms such as: sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest.
Anti-anxiety medication: These types of medication are used to treat GAD and panic disorders. They may also help with insomnia and agitation. They are a type of antidepressants. They can be fast-acting and can help with short term relief, but these types of drugs have the potential to cause dependency, so it is recommended that they be used shirt term only.
Mood-stabilising medications: These are most commonly used for bipolar disorders. This involves alternating episodes of mania and depression. Sometimes these drugs are used together with antidepressants.
Antipsychotic medications: These are the hard core drugs used for psychotic disorders such as schizophrenia. They can also be used for bipolar disorders or used with antidepressants to treat depression.
Self care: research indicates that physical activity has benefit across ages and levels of illness. The benefits are of particular reference to those who have depression.
Brain stimulation treatments: can be used for depression and other issues. These are generally used when medications and psychotherapy have not worked. They include electroconvulsive therapy, repetitive transcranial magnetic stimulation, deep brain stimulation and vagus nerve stimulation. There are risks with these electrical stimulation therapies.
Hospital and residential treatment programs: sometimes people need institutionalisation when mental illness becomes severe. This is recommended when the person is in danger of self harm. The time frame can be anything from 24 hours to specialised time frames. Or the person can obtain outpatient treatment.
Substance misuse treatment: quite often, in order to alleviate the constant barrage of mental pain, people often take recreational drugs or excess alcohol. However, this interferes with treatment and worsens mental illness.
Employee Assessment Programs: in the workplace many companies have opted for an online assessment option whereby employees can self assess and then avail themselves of external treatment with a therapist who is aligned with that program. Theoretically is anonymous. However, many employees are wary of these programs as they do not want to be labelled as having mental health issues. Or, in the worst case scenario, they do not want to become trapped within the mental health system and be registered on some list whereby they have to take prescribed psychotic drugs on an on-going basis, or forever. And. That is why employees are wary of these programs and that even though a minimum of 26% of employees are severely depressed, the uptake of these programs, hovers between 5 – 7 %.
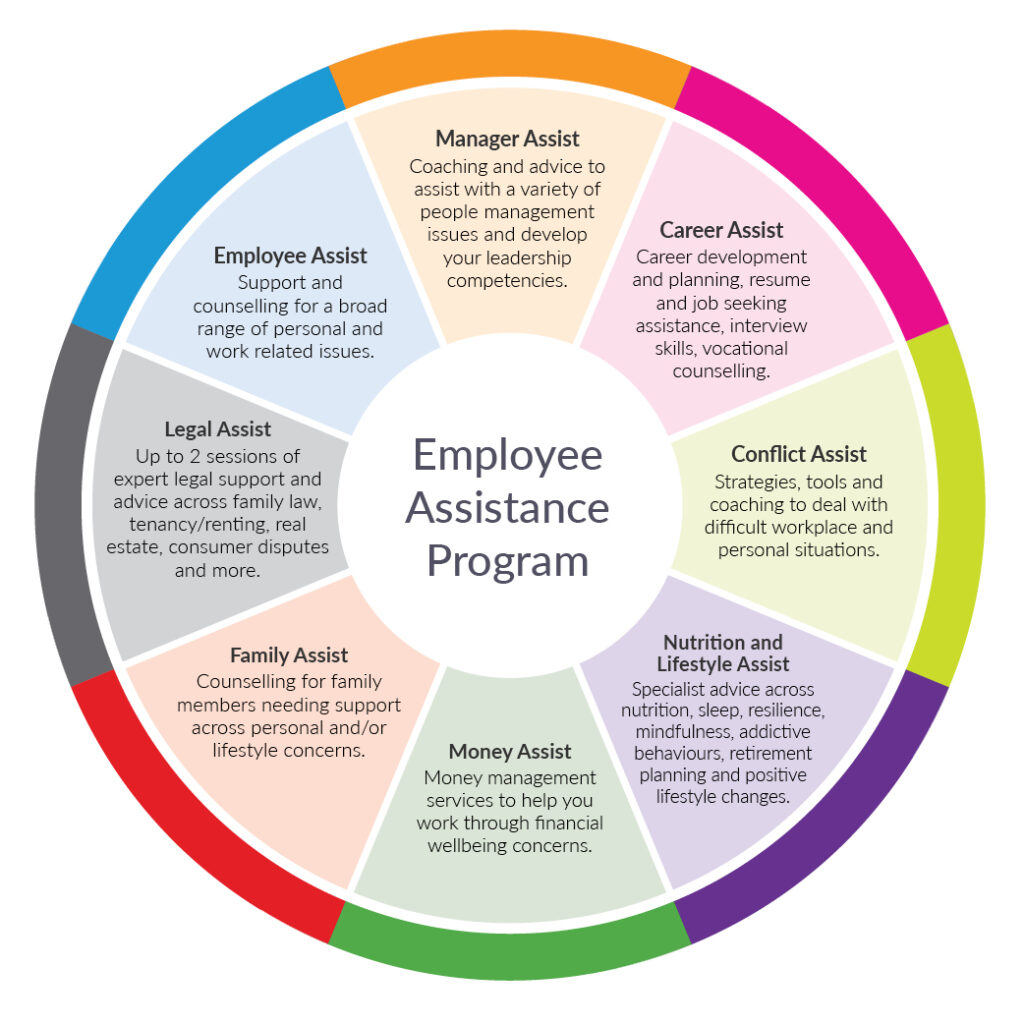
The scepticism that arise from EAP type of programs include:
- Suspicion that they are not confidential
- The employees feel that there is stigma attached to reaching out for help
- They think they have to ask permission from their boss or HR
- Or, they do not know that these EAP’s exist, are available for all, and do not cost the employee anything
So, how do you overcome these fears?
- Educate employees that the information is confidential
- Normalise problems everyone has issues
- That employees need to know that you do not need to ask the boss or HR to undertake an EAP or the resulting external counselling available
Lifestyle and home remedies: it is recommended that professional help is used as a starting point. However, there are some things that individuals can do to help themselves:
- If you have a plan then stick to it with the professional treatment and sessions with a counsellor or psychotherapist
- Avoid alcohol and drug use
- Stay active – any kind of mild exercise will help
- Make healthy lifestyle choices – sufficient sleep, eating health food, keeping positive, surrounding yourself with supportive people
- Avoid making big decisions until you have improved
- Reduce obligations and determine your immediate priorities instead of becoming overwhelmed
- Learn to adopt a positive attitude
In summary: all treatment is base on the notion that without help, mental health issues will get worse. The first point of call is always your family doctor. From there he/she will prescribe basic treatment. If things do not improve then the doctor will refer you to more specialised help. Further help generally will comprise talking therapies and medication. IN the workplace employers have instigated EAP’s to try to help employees self-assess with mental health issues. However, it appears that, so far, these programs have not been fully successful.
7. A New Perspective on Dealing With Employee Mental Health Issues in the Workplace- Let’s Talk About Stress Reduction
As alluded to earlier, stress is the basis of all of our reactive thoughts, behaviours and emotions. The word: “reactive” was originally contained in earlier version of the DSM bibles of classified mental health disorders, then it was removed.
Why?

Probably because it was too hard to stipulate what the outcomes might be from that reactions, because, in theory, everyone may have a different reaction to a set of circumstances. And. These will be based on: early childhood environment, experiences of their primary care-givers, the interpretations of experiences individuals have had, and the role-modelling behaviour of these primary care givers, the perceptions built and the negative beliefs underpinning these perceptions have led to how people react, and behave and think and feel when re-experiencing those events later in life.
Because these experiences and the related emotions are stored in the body/mind, we do not know when these memories will be triggered, and therefore, such “reactions” cannot be classified, succinctly.
So, what this means is that in order to be able to classify mental health disorders more easily, “reactions” to events simply cannot be classified, and therefore, can only be exposed during counselling sessions.
My theory is that all dis-ease and disease stems from stress. (The basis of this opinion is scientific research, particularly form Dr Bruce Piton, eminent biologist, in his book titled: The Biology of Belief, who stated that up to 95% disease is stress-related and that this means that the individual is creating these diseases.)
This means that individuals have stored memories of past events within their body/mind. These memories have energy attached. When a stressor trigger is activated by an event that appears to be similar to a past stored memory, this then leads the individual to react in certain ways, ways that he/she decided was a useful, and appropriate coping mechanism at that time. (It may not be now. However, the individual’s emotional brain does not know this)
So, this means that this old behaviour, thought and emotional patterns of reaction are still being played out, unbeknownst to the individual. Also, too, we also have the situation with political correctness, together with being put down for espousing opinions on anything that might be construed as: racist, ageist, sexist or fascist, that people do not express themselves for fear of being outed and ostracised.
In the workplace it is not politically correct to tell your bosses what you think, nor how you feel, especially if you feel you are not coping. Why? Because if you do, you will be considered weak, ineffective or have some kind of stigma attached, especially if you acknowledge that you might be have feelings of depression or anxiousness.
The result? Suppression of expression. And. What does this lead to? Depression. When you are unable to express your opinions, your values, your ideas in safety, you suppress these thoughts. This will lead to dis-ease within the body/mind and eventually disease, if not treated appropriately.
For those who have a tendency towards anxiety, this will mean that you feel that you are unable to control various factors around you at work and therefore you will spend more and more time at work trying to keep on top of things, in order to hide those anxious feelings.
So, in both instances: anxiety and depression disorders, especially in the workplace, you will find employees dulled down. They want to keep their jobs. They fear being singled out for non-performance issues. They fear stigma.
So, in essence, the key to relieving employee mental health issues in the workplace, is to deal with the underlying issues that cause reactions to certain events. This is a personal thing. For a comprehensive overview of how stress affects every aspects of our lives see The Ultimate Guide To Letting Go And Moving On (In 2019)
From a practical point of view, a more acceptable way to address employee mental health in the workplace, is by addressing it from a stress reduction point of view. Why? Everyone is affected by stress. So, those people who are experiencing depression or anxiety will be lumped into the pool of stressed employees, and not singled out as those who are experiencing mental health issues. P
The key now is to work out how this might work – introducing a stress reduction-based program into the workplace that deals specifically with all kinds of issues, but which also addresses depression and anxiety. point
In summary: the new perspective is to view employee mental health issues as stress-based issues, which they are. Studies have indicated that 87% of employees are depressed (or anxious), So, the better option could be to offer a more inclusive approach, instigating company-wide stress reduction programs to deal with the many kinds of mental health problems employees may have. This in turn would deal with depression and anxiety, by default. of view,
8. A New Solution: A Five Step Stress Reduction Plan for Leaders to Help Employees Deal with Mental Health Issues in a More Comprehensive Way
All stress resolution programs revolve around boosting energy and changing negative energy, lack of focus and concentration into positive attributes. If you are feeling depressed or anxious, you are focusing on issues that have negative beliefs and emotions attached. You are relieving these stories over and over and creating havoc in your body/mind.
So, how do you go about changing those patterns of thinking, behaviour, reactions, beliefs and negative emotions?
You have to retrain the body/mind accordingly.

Since stress is the basis of all disease, it means that you simply must change how you respond to stress, as a better coping strategy. And. Yes. You can learn to do that with very successful results.
In my article titled: How To Boost Energy – A Wellness Plan – Your Must Have Wellness Formula Ingredients you can read about this in detail.
The new Five Step Stress Reduction Plan to overall wellness from employee mental health issues in the workplace outlines in these five steps:
1. REPAIR – your physiology
2. RELEASE – the negative beliefs underlying those issues which are the real cause of these mental health issues
3. RENEW – the body/mind – right down to the cellular level
4. RECREATE – whereby you uncover your true identity, your innate skills, talents and abilities, so that you will be able to express who you are at that level, and therefore make your contribution to the planet, and
5. RECLAIM – whereby the individual can then set meaningful goals, goals which will be aligned with your true identity.
The initial programs offered in companies and organisations revolve around changing how you respond to stress. When this happens, individuals gain control of patterns of thought, behaviours and emotions and can then retrain themselves to come from a positive point of view rather than coming from an automatic negative point of view.
The programs used world-wide by thousands of people over a long period of time, have seen these types of results:
- 60% decrease in depression
- 30% improvement in sleep
- 46% decrease in anxiety
- 24% improvement in focus and
- 50% decrease in fatigue
If these results are available from specific stress reduction type programs why aren’t management implementing them?
The only logical reason is because they are not aware that they are available.
For a detailed expose on what is available please download this document titled: Is Your Organisation a Productive and Happy Place for You and Your Staff? – The Cost of Workplace Stress in Australian Organisations at: FREE Resources – Celine Healy Consulting
9. Some Commonly Asked Questions on Employee Mental Health such as: What causes mental illness; Can mental health go away… and other questions?
When individuals experience dis-ease or have symptoms that are worrying the first place they go is to Dr Google. Generally, the questions are short and the answers are even shorter, just to give the person sufficient information to see if they need to delve further.
In this section we will look at some of these commonly asked questions on mental health and employee mental health, in particular.
We have dealt with the history of mental health and some background previously, we will not delve into those questions here. You can read them in the relevant sections above.
Commonly asked questions on mental health issues
a. Generally, what age do mental health issues start?
Due to the changing nature of our society and the advent of social media we have seen that the age has decreased. 50% of mental illness begins by the age of 14. 75% begins by the age of 24, and this is evident also by the numbers of suicides of young men under 24 years of age. Psychotic illness such as: schizophrenia or bipolar rarely appear out of the blue. They develop over time.
The more worrying information is that there is a significant number of children under the age of 10 with depression, anxiety and all manner of ADD and ADHD type issues who are prescribed Ritalin and other mood-altering drugs. The other worrying trend is “eco-anxiety” experienced by children who feel threatened by climate change alarmist propaganda.
b. Briefly, how is mental health treated today?
The preferred method of treatment is psychotherapy combined with medication. This is to avoid the last resort option of psychiatry and institutionalisation. The types of therapy include: cognitive behavioural therapy, exposure therapy, dialectical behaviour therapy and others. The approach is to try “talking:” therapies as a first option.
c. What causes mental illness?
The commonly held belief is that mental illness evolves from a number of factors including physical, emotional as well as psychological. Modern day thinking has evolved to add that these illnesses may be caused by a reaction to environmental stresses, include genetic factors, be due to biochemical imbalances, or a combination of these factors.
I personally believe that stress is the basis of ALL mental illness, and, that if the underlying issues that cause the stress reactions are not dealt with then mental illness will be exacerbated, and hence increase.
d. Can mental illness go away?
This depends on the level and degree of incapacity. If the mental illness has progressed to a psychosis then it is harder to decrease. If the mental illness is in the early phases of depression and anxiety then there is very good reason that these can be remedied with a combination of treatments. In all treatment plans the person needs to address the underlying stress issues. They also need to make sure that physiological factors such as nutrition, supplements, food and exercise need to be actioned.
e. Can mental health be cured?
Most practitioners feel that the symptoms can be reduced with appropriate treatment. Up to 95% of all illnesses are self-inflicted. If that is the case, then surely, they can be self-cured. However, this takes enormous time and effort. I personally believe that in the early stages ALL disease can be cured/reversed. However, once the synapses of ill health are ingrained deeply, coming back from that position, takes super-human effort.
f. Who is at risk for mental health illness?
The risk factors include: a blood relative having these types of illnesses, stressful life situations, on-going physical health issues, lack of support and resources to be able to instigate self-help.
g. What are the factors that affect mental health?
Generally, the types of factors include self-image and life experiences that impinge on the psyche of an individual:
- Self esteem
- Feeling loved
- Confidence
- Family break-ups or loss
- On-going difficult behaviour issues
- Physical ill health
- Abuse – emotional and sexual and domestic violence issues
h. What type of mental illness might I have?
There are many different categories. However, the most common types are: depression, anxiety and psychotic illnesses.
Depression can be treated by your family doctor in the early stages. Anxiety can also be treated by your physician. However, psychotic illnesses need specialised treatment. Your first point of contact would be your family doctor.
i. Will talk therapy help?
There have been many instances of “talk therapy” helping some people. I personally believe that a person needs to be able to release the underlying negative beliefs first, in therapies such as hypnosis or kinesiology, before any meaningful “talk therapy” can take place. Why? Because many people are ill-equipped to talk through issues especially when they do not feel that they have any control over their lives. Gain control first. Then talk afterwards.
j. How long will treatment take?
If you have been abusing your body/mind for years then expect that it will take some time to restore normality. The best first step is to start to repair your physiology. You will need to eat well, take supplements, rest, sleep well and exercise, and take time out. There is no set time limit on this.
In summary: mental illness does not suddenly appear. The build-up to exhibiting symptoms can take years. If you are trapped within cycles of negative thoughts, behaviours and feelings, then you will also need to retrain your mind, to come from a more positive position. Most people will not be able to do this themselves and will require a treatment plan. You can start this with your doctor. If after a reasonable period of time your symptoms do not improve then you will need to seek a more clinical approach. This may involve talk therapy and medication.
10. A Challenge to Leaders: Implement Real Change on Employee Mental Health Issues or Continue Following the Pack?
The challenge for leaders is to take notice of the results of the EAP uptake by employees in your organisation.
If we know that 87% of workers are depressed (and anxious) from mild, medium and severe, this then means that there is a real issue here.

If we know that the uptake of EAP’s is between 5-7%, this then means that there is an issue with employees’ trust in management to keep their results confidential. If and when employees put up their hand to say that they need help, what and how will management convey to their staff that the information will be confidential, and that they will not suffer with ostracization or stigma.
It is obvious that employees do not trust management/leaders with their personal mental health issues. They feel they are not able to discuss this easily and confidentially.
My solution is that employee mental health issues need to be addressed from a different perspective. Firms need to treat everyone equally and introduce stress reduction programs instead, so that everyone is included, and the small minority is not singled out. In this way real progress will be obtained. and everyone will be able to help each other out.
Way forward
Employee mental health issues are increasing world-wide and are rampant even though companies have tried to solve the issues with the implementation of Employee Assessment Programs.
A solution has been offered, via approaching the issue from a different angle – that of reducing stress. This does work and has been scientifically proven. Research indicates that stress in the workplace is of real concern.
The challenge to leaders is: do you want to implement real change or do you take the easy path and continue with programs that staff view with suspicion?
In all cases early treatment needs to be instigated, so that improvement in symptoms can be effected.
As a leader – what will you do?
If you have enjoyed this topic please leave your comments below.
About the Author: Celine Healy is a speaker, writer, blogger, and a trainer on topics such as: stress, wellness, leadership and corporate well-being. Celine is also passionate about mental and physical health. Celine approaches these topics from a scientific point of view. “If you can’t measure something, you will never understand it.”